Analyse & Respond To Client Health Infomation Essay
Analyse & Respond To Client Health Infomation Essay
Q1) Diabetes Type 2 is the most common form of diabetes where the pancreas can still produce insulin however the body loses the ability to use the insulin it produces effectively, this is called insulin resistance, (“Type 2 diabetes”, 2018). Cells don’t respond to insulin and the pancreas does not produce enough insulin for the body’s increased needs. If the insulin cannot do its job, the glucose channels do not open properly.Analyse & Respond To Client Health Infomation Essay. Glucose builds up in the blood instead of getting into cells for energy. Type 2 diabetes results from a combination of genetic and environmental factors. Although there is a strong genetic predisposition, the risk of developing type 2 diabetes is significantly increased with factors that may be related to lifestyle choices including high blood pressure, high cholesterol and insufficient physical activity.
Q2) Poor blood circulation or loss of sensation due to diabetes-related nerve damage means that pressure on the skin goes unnoticed resulting in pressure ulcers. This also links back to Percy’s past medical history of peripheral neuropathy. It is the inability of the damaged skin to repair itself normally that result in ulceration.
Q3) Percy’s BGL recorded 2. 7 mmol/l. This means his hypoglycaemic. I would get him to drink a soft drink or something with sugar in it. Then I would continue to check his BGL over the next 5 hours.
Q4) Percy’s wound is red and leaking fluid because it’s infected. Diabetes reduces the blood circulation to and around the wound site. A lack of circulation in the extremities can result in a reduced supply of oxygen and nutrients to the body tissue and nerves, which is necessary for healing. Over time, nerves in these areas may become damaged, decreasing the sensation of pain, temperature and touch, making patients vulnerable to injury.
Q5) Endocrinologist An endocrinologist is a medical specialist who is trained to diagnose and manage diseases that affect the glands and the hormones. An endocrinologist aims to restore hormone balance within the body’s systems. Endocrinologists commonly treat and provide expert advice on the management of diabetes. Die titian A dietician will work with the patient to develop a personalised healthy eating plan to suit their lifestyle, their type of diabetes and individual health needs. They can educate on how to read food labels, modify recipes and even how to order at restaurants to make healthier choices. Exercise physiologist/physiotherapist An exercise physiologist/physiotherapist can help to determine the appropriate exercise/activity plan for the patient individually suited to their needs and lifestyle. They will assist in increasing mobility and comfort.
ORDER A PLAGIARISM-FREE PAPER NOW
Case Study two – Neurological and urinary disorders
Q6) Urinary Tract Infection due to positive levels in protein, nitrates and blood.
Q7) Risk factors for urinary tract infection include
- duration of catheterization – insertion
- aphasia – patients inability to speak makes it harder for her to alert physicians of burning sensation and pain when voiding
- CVA – stroke severity, depressed conscious level increased post-void residual urine volume. Analyse & Respond To Client Health Infomation Essay.
Q8) “Fever is generally defined as a temperature above 38 degrees, and occurs when the hypothalamus increases the core body temperature in response to an infection” (Musselman & Saely 2013). Febrile temperatures operate as a systemic alert system that promotes immune surveillance during challenge by invading pathogens, (Koutoukidis, Stainton & Hughson, 2017)
Q9) TIA (Transient Ischaemic Attack) – occurs when the blood supply to the brain is blocked temporarily. When the blood supply is stopped, the brain cells in the area start dying, and you experience signs that something is wrong, (“Transient ischaemic attack (TIA) — Stroke Foundation – Australia”, 2018). The signs and symptoms are similar to that of a stroke however they disappear within a short time and are often only present for a short time. After a TIA the risk of having a stroke is higher and often acts as a warning sign. CVA (Cerebrovascular Accident) – often referred to as a stroke. A stroke is a sudden loss of cerebral circulation, which causes cerebral infarction. The sudden death of some brain cells due to lack of oxygen when the blood flows to the brain is impaired by blockage or rupture of an artery to the brain. An embolic stroke occurs when a blood clot that forms elsewhere in the body breaks loose and travels to the brain via the bloodstream. When the clot lodges in an artery and blocks the flow of blood, this causes an embolic stroke.
Q10) Neurologist: This doctor is a specialist trained to treat disorders that affect the brain, spinal cord, and nerves, such as: Cerebrovascular disease, such as stroke. Speech Therapist: This professional helps you relearn language and communications skills. Speech therapists also help you deal with swallowing problems and develop alternative ways of communicating. Physiotherapist: uses exercises and physical manipulation of your body to help restore movement, balance and coordination. Physiotherapists can help you relearn movement skills, such as walking, sitting, lying down and switching from one type of movement to another. Case Study three – Respiratory, genetic and reproductive disorders
Q11) ‘Cystic fibrosis is inherited as an autosomal recessive condition’, (“Cystic Fibrosis – What is CF”, 2018), this means a child can only have the disease if both parents are carriers. Carriers have no symptoms; however they do carry a genetic change referred to as a “mutation” that may be passed on to future generations. Because Madeline’s parents are both carriers there is a 1 in 4 (25%) chance that both passed on the non-functioning gene, (“Cystic Fibrosis – What is CF”, 2018).
Q12) Cystic fibrosis causes the mucus that coats the bronchial tubes to become so thick and sticky that the cilia are unable to sweep the germs and other particles up and out of the lungs. The trapped bacteria lead to frequent, serious infections and permanent lung damage.
Q13) Most men with cystic fibrosis are infertile because of a blockage or absence of the sperm canal, known as congenital bilateral absence of the vas deferens (CBAVD). Analyse & Respond To Client Health Infomation Essay. The sperm never makes it into the semen, making it impossible for them to reach and fertilize an egg through intercourse. The absence of sperm in the semen can also contribute to men with CF having thinner ejaculate and lower semen volume.
Q14) Madeline will experience exacerbation of respiratory and other disease symptoms, requiring intensified treatments, if she decides to fall pregnant. Normal pregnancy is associated with significant respiratory, cardiovascular and metabolic changes. Although healthy women usually adjust easily to these changes, they may impose a considerable strain for women whose physiology is already severely compromised with cystic fibrosis.
- Increased risk of pulmonary infection
- Decreased pulmonary function
- Increased oxygen consumption
Q15) Pulmonologist: managing the care of chronic respiratory diseases is one of a pulmonologist’s main duties. Pulmonologists also coach their patients on management of their illness, by making lifestyle changes or learning coping strategies to minimize their reliance on medications.
Respiratory Therapist: performs pulmonary function tests to measure the air flow and volume in your lungs. Assists with pulmonary therapies, which are designed to clear mucus (sputum) out of your lungs, control bacteria and reduce the inflammation of your airways. These therapies involve airway clearance techniques (ACTs) and inhaled or nebulized medications.
Physiotherapist: Physiotherapy management is a key element of care for people with cystic fibrosis. The lungs make mucus to help defend against germs. Cystic fibrosis changes the mucus, making it thick and hard to clear. Brisk percussion of the chest wall helps to break up and dislodge mucus, so it can be more easily coughed out of the body.
By the end of this chapter, we would like you:
-To explain the place of health observation and assessment in the nursing care cycle.
-To list and describe the three key steps involved in health observation and assessment.
-To explain the difference between signs (objective) and symptoms (subjective).
-To describe the application of clinical judgement to understand assessment data.
-To discuss cultural considerations related to health observation and assessment.
-To describe the processes involved in conducting a systematic head-to-toe assessment of a patient, including completing a primary survey and a secondary survey. Analyse & Respond To Client Health Infomation Essay.
-To be able to accurately document health observation and assessment findings.
Health observation and assessment in nursing practice
| Health observation and assessment is a systematic process to collect data about a patient. This data provides information about the patient’s condition, and is used to inform the care which is appropriate for that patient. Nurses undertake health observation and assessment constantly, in all clinical settings.
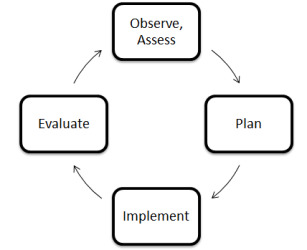
Health observation and assessment is the first step in the nursing care cycle, illustrated in the diagram to the right: |
 |
Health assessment involves three concurrent steps:

- Health History: collecting subjective data – data about a patient’s symptoms. Data is collected via an interview with the patient and / or significant others. Data collected may be primary or secondary.
- Physical Examination: collecting objective data – data about a patient’s signs. Data is collected via a physical examination of the patient, using techniques such as inspection, palpation, percussion and auscultation, and measurement of the vital signs and other key physical indicators.
Symptoms are what the patient subjectively experiences. Signs are what a nurse objectively observes, feels, hears or measures. In some cases, data collected during health observation and assessment may be both a symptom and a sign. For example, a client may say that she “feels sweaty” (a symptom), and the nurse observes diaphoresis (a sign).
- Documentation of Data: data collected during health observation and assessment must be documented so that it can be used to: (1) assess the patient’s condition, and (2) inform the care which is appropriate for that patient. There are a variety of ways that data can be recorded. Regardless of the manner, documentation must be complete, accurate, concise, legible and free from bias.
There are a number of different types of health assessment which a nurse may undertake:
- Comprehensive health assessment: taking a detailed health history and physical examination of a client, to identify all of the person’s health care issues and needs. Usually performed on admission.
- Problem-based / focused health assessment: collecting data related to a specific complaint. Common in outpatient settings.
- Rapid assessment: collecting data to provide immediate, life-sustaining intervention to a patient. Often performed in emergency care. Analyse & Respond To Client Health Infomation Essay.
- Episodic / follow-up assessment: a nurse following up with a patient to collect data on a previously-identified problem. The goal is to determine how the patient has responded to care, by identifying changes in the patient’s condition.
- Screening assessment: collecting data with the aim of detecting the presence of a specific disease.
The type of assessment used depends on: (1) the context, and (2) the health care issues and needs of the patient. In an acute care setting with a new client, a comprehensive health assessment is usually appropriate. However, in an emergency care setting where a patient presents with a clear, significant problem, a rapid assessment is typically more suitable.
Cultural considerations in health observation and assessment
A person’s culture is far more than simply their ethnic background; it involves how they live in and perceive the world around them. People who share a culture also share values, beliefs and attitudes about various topics – including about their health. Nurses have the responsibility of providing effective care to people whose health practices, values, beliefs and attitudes may differ significantly from their own.
It is important that nurses are respectful of a diverse health practices, values, beliefs and attitudes. This involves, in part, becoming a culturally competent nurse.
Nurses are not expected to know all the health practices, values, beliefs and attitudes of all the different cultural groups they work with. They should also avoid stereotyping the people with whom they work. Rather, nurses must recognise each person as an individual. Nurses are encouraged to ask questions to understand the patient’s health practices, values, beliefs and attitudes.
Conducting a systematic head-to-toe assessment and primary / secondary survey
This chapter introduces the idea of a ‘head-to-toe assessment’, a physical examination which enables a nurse to assess a client systematically and comprehensively from the top of their body downwards. When conducing a head-to-toe assessment, nurses assess each body system in turn, to develop a detailed overall understanding of the patient’s condition.
Each nurse’s approach to completing a head-to-toe assessment is unique. The only requirement for a head-to-toe assessment is that the process is systematic and comprehensive, and that no data is omitted.
Head-to-toe assessment begins with observation. The nurse should observe the patient, noting their gait, posture and ease of movement, communication ability, physical appearance and general mental alertness / orientation / thought process.Analyse & Respond To Client Health Infomation Essay. This is to identify any obvious problems which may need to be addressed assessment can begin, or which may inform the focus of this health assessment.
Once a nurse has completed their observation of a patient, they can progress to completing the head-to-toe assessment. This is done in two parts:
- The primary survey, which involves assessing the patient’s life-sustaining body systems.
- The secondary survey, which involves a more comprehensive assessment of the patient.
The primary survey involves four stages, which may be remembered using the ‘ABCD’ mnemonic:
| A | Airway | This step involves assessing the patency of the airway. A nurse should observe the patient for dyspnoea, excessive upper respiratory secretions, respiratory problems such as coughing / choking, and airway trauma, etc. | ||||||||
| B | Breathing | This step involves assessing the adequacy of the patient’s breathing and gas exchange. The nurse should observe the patient for dyspnoea, paradoxic or asymmetrical movements of the chest wall, accessory muscle use, changes in breath sounds, cyanosis, tachycardia, etc. | ||||||||
| C | Circulation | This step involves assessing the functioning of the cardiovascular system and whether the patient has adequate blood volume. The nurse should assess the quality and rate of the pulse, capillary refill time, and skin colour and temperature. | ||||||||
| D | Disability | This step involves briefly assessing the patient’s neurological system, including their level of consciousness. Another simple mnemonic – ‘AVPU’ – is used to prompt nurses during this step:
During this step of the primary survey, other disabilities – for example, obvious physical or psychological problems – may also be identified. |
The vital signs should also be measured and recorded. The nurse can then progress to the secondary survey. This involves using four key techniques: Analyse & Respond To Client Health Infomation Essay.
- Inspection – assessing a part of the body by observing it.
- Palpation – assessing a part of the body by touch. The nurse may use their palmar surfaces and finger pads to determine position, texture, size, consistency, masses, fluids, crepitus, pulsations, etc.
- Percussion – assessing the contents of a space in the body by tapping it with a finger. Percussion is undertaken to evaluate the size, borders and consistency of the internal organs, to identify tenderness, and to detect the presence of fluid in a body cavity. When percussing the body, the nurse should expect to hear the following sounds:
| Area Percussed | Normal / Expected Sounds |
| Lungs | Resonant tone; loud intensity; low pitch; long duration; hollow quality. |
| Bone, muscle | Flat tone; soft intensity; high pitch; short duration; extremely dull quality. |
| Viscera, liver | Dull tone; medium intensity; medium to high pitch; medium duration; ‘thud-like’ quality. |
| Stomach, gas in intestines | Tympanic tone; loud intensity; high pitch; medium duration; ‘drum-like’ quality. |
| Air trapped in lungs (e.g. in emphysema) | Hyper-resonant tone; very loud intensity; very low pitch; longer duration; booming quality. |
- Auscultation – listening to sounds.
The nurse should assess:
| Body Region | Examples of Health Observation and Assessment |
| The head and face |
|
| The eyes |
|
| The ears |
|
| The nose, mouth and oropharynx |
|
| The neck |
|
| The upper extremities |
|
| The posterior chest |
|
| The anterior chest |
|
| The abdomen |
|
| The lower extremities |
|
| The neurologic system |
|
| The genitalia and rectum
(if indicated) |
|
It is important that nurses comply with their organisation’s policies and procedures. In order to perform an assessment using a particular technique, it is also important that nurses are appropriately trained in the correct use of that technique, and in the data it returns.
There are a range of other focused assessments which may also be completed – for example:
- Blood glucose levels.
- Blood laboratory studies.
- Comprehensive neurological evaluation.
- Diagnostic imaging studies.
- Electrocardiogram (ECG) monitoring.
- Height, weight and Body Mass Index (BMI).
- Mental health assessment.
- Neurovascular function.
- Pain assessment.
- Sensory perception.
- Skin assessment.
- Urinalysis.
It is important that nurses are familiar with any pieces of equipment which may be used in the assessment of a patient. This equipment may include (but is not limited to):
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
When assessing a patient, it is important that you are organised and prepared with the equipment you need. It is important that you develop a routine, and that you practice this so you develop confidence.
Documenting health observation and assessment findings
At each stage of the assessment, it is important that nurses document, or record in written format, the data they collect. This allows data to be: (1) used to determine the patient’s clinical condition and make decisions about appropriate care, and (2) communicated between different professionals involved in the care of the patient. Analyse & Respond To Client Health Infomation Essay.
ORDER A PLAGIARISM-FREE PAPER NOW
There are a variety of different ways that data can be recorded, and this differs between clinical settings and organisations. Regardless of how data is recorded, however, documentation must:
- Be complete, accurate, concise, legible and free from bias.
- Record facts, without the use of non-committal language.
- Be written contemporaneously, or as close to the time of collection as possible.
- Include the name, signature and designation of the nurse who created it.
- Be unaltered; if errors are made, these must be struck through with one line and initialled.
- Be kept securely, an in a way which protects the patient’s right to confidentiality.
- Avoid using acronyms, abbreviations, jargon and archaic terms.
- Use short sentences and simple words.
- Involve the patient and their significant others, and use language they understand.
As stated by the National Health Service’s (NHS, 2010: p. 2) CG2 – Record Keeping Guidelines, “[r]ecords must demonstrate a full account of the assessment made, the care planned and provided and actions taken, including information shared with other health professionals.”
Creating and maintaining appropriate documentation is a legal, ethical and professional requirement for nurses. Health records provide evidence about the type of assessment and care patients receive. They are also important clinical tools, enabling continuity of care and effective decision-making.
Conclusion
This chapter has provided a broad introduction to health observation and assessment. It began with an overview of health observation and assessment. The processes involved in conducting a head-to-toe assessment, including a primary and secondary survey, to collect data from a patient in an accurate, comprehensive and systematic way have been described. Finally, this chapter described the correct documentation, or recording, of data collected during health observation and assessment. Analyse & Respond To Client Health Infomation Essay.
