Promoting Health and Preventing Ill Health Essay Paper
Promoting Health and Preventing Ill Health Essay Paper
Introduction
Asthma is a common chronic childhood respiratory disease characterized by narrowing of the airways and swelling and overproduction of mucus (Miraglia et al., 2014). A child with asthma will tend to exhibit common symptoms like wheezing, shortness of breath, coughing, and tightening of the chest. The symptoms may, however, be erratic depending on the variations in their levels of severity, frequency, and duration of occurrence. It is also typical for the symptoms to differ from one child to the next, although this does depend on whether their asthma can be classified as either severe or mild. Whatever the case may be, long-term conditions could be effectively managed. In this paper, McGill Nursing Model is applied to develop a nursing plan to delineate treatment of asthma in a 12-year-old child who has just been diagnosed with this chronic disease (Doenges et al., 2019). The goals of this care plan are to control the inflammation in an asthmatic child’s airways and to eventually minimise his exposure to substances known to trigger wheezing, shortness of breath, coughing, and tightening of the chest. The expected outcome includes making sure that the child’s airways facilitate normal respiratory processes.
Asthma Risk Factors
The common risk factors for childhood asthma development include having an asthmatic parent, the onset, and development of a serious respiratory infection, exposure to some allergens or chemical irritants, and having an allergic condition (Ahmed et al. (2016). Promoting Health and Preventing Ill Health Essay Paper
What puts children at risk for asthma development include:
- Family history – research has shown that children who have a parent with asthma are particularly at risk of developing asthma in comparison to those who do not have an asthmatic parent (Bhattacharjee et al., 2018).
- Severe respiratory infections – Children experiencing severe respiratory disorders are more at risk for wheezing. When wheezing persists for weeks or months, the children may eventually develop chronic asthma.
- Allergies – Children with allergic conditions, with a common one being eczema (atopic dermatitis), or hay fever (allergic rhinitis), are particularly at risk for asthma development (Ahmed et al., 2016).
- Environmental exposure – Children who are frequently exposed to certain dust in their environment, such as chemical vapours, fumes, or moulds are also at risk for asthma development. Similarly, when children are exposed to components of smog (ozone), they become more at risk for asthma development. This is normally the case when a child lives in urban areas that are frequently susceptible to smog (Bhattacharjee et al., 2018).
- Smoking – Cigarette smoke is more likely to irritate children’s airways through second-hand exposure. At the same time, children whose mothers were exposed to second-hand smoking during their pregnancy or even smoked during this time are more likely to develop asthma (Bhattacharjee et al., 2018).
- Obesity – Children who are obese or overweight have also been found to be at a greater risk of developing asthma. While the reasons remain vague in research, some researchers have identified low-grade inflammation occurring in children with extra weight as putting them at risk of asthma (Mohanan et al., 2014).
ORDER A PLAGIARISM-FREE PAPER HERE
Although it could be discerned from current research that the above-mentioned factors increase children’s risk for developing the conditions, several other factors that have been linked to asthma development include poverty, because of incapacity to seek for diagnosis, medication, and hospitalisation (Bhattacharjee et al., 2018).
Pathophysiology
Asthma can be described as a chronic airway condition that is normally characterised by pieces of evidence of an inflamed airway, persistent hyper-reactivity of the obstructed air ducts and, and obstructed air ducts. These conditions have complicity in the occurrence of the tightened chest, shortened breath, coughing, and wheezing. Overall, asthma can then be identified by bronchial hyper-responsiveness, which is a condition whereby an overstated response of the airways occurs usually triggered by inflammatory allergens and cytokines (Barnes, 2006).
Airway inflammation: Airway inflammation occurs when the cells and tissues in people who have asthma become sensitive to inflammatory reactions to allergens or irritants that would, in normal cases, be risk-free. Typically, airway inflammation sets off mucus production and airway contraction (Bhattacharjee et al., 2018).
B-cells produce immunoglobulin E (IgE) antibodies that prompt discharge of inflammatory mediators like histamine and leukotrienes, which are found in the mast cells. The two are responsible for causing constriction of the normally smooth muscles.
Airway remodelling: Bronchial tubes may be damaged by chronic and usually uncontrolled asthma attacks, which trigger the shedding of epithelial cells. The implications of this remodelling of the airway include permitting infiltration of irritants and allergens to travel further into the interior muscle cells (Bhattacharjee et al., 2018).
Signs and symptoms
Symptoms of asthma include:
- Coughing frequently and in short intervals at night
- Sleeping difficulties
- Frequent wheezing
- Shortness of breath
- Tightening of the chest
- Frequent fatigues
- Rapid breathing
- Running nose, sneezing, headache, and congestion of the nostrils (Bhattacharjee et al. 2018).
While it is typical for these symptoms to persist, not all children with asthma may show the same kinds of symptoms (PICS, 2013). Even as some patients may take longer periods without indicating the abovementioned symptoms, some are likely to experience asthma while taking part in vigorous physical activities whenever they are exposed to viral infections like common cold or flu. Mild asthma attacks tend to be more prevalent than severe ones, and are normally typified by the opening up of the airways for a few minutes or even hours. Severe asthma attacks tend to take longer (Bhattacharjee et al., 2018).
Health History
As recommended by McGill’s Nursing Model, it will be necessary to review the history of the child’s health. However, this will need to be undertaken in collaboration with the parents of the child, or if applicable members of his family or a guardian. Promoting Health and Preventing Ill Health Essay Paper The specific areas that will be looked into include whether the symptoms of the child happen more recurrently in fall or spring. It will also be necessary to find out from the child’s parents if the symptoms are set off by respiratory infections, exposure to cold weather, or physical exercises. It will also be important to inquire from the parents whether there is a family history of the condition, as well as other condition like eczema and hay fever (Bhattacharjee et al., 2018).
Assessment
Classification of asthma will be determined depending on the level of its severity. To classify the client’s asthma severity, the focus will be placed on the child and her parents’ answers to questions regarding symptoms. The questions will centre on the frequency of asthma attacks the client experiences, and how long they take on average. The focus will also be placed on examining the results of diagnostic tastes and physical exam.
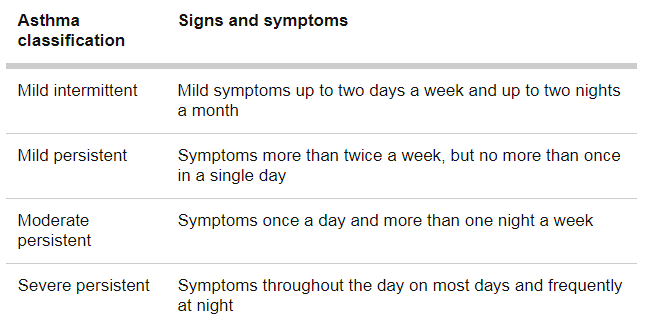
Establishing the severity of the asthma is critical, as it will assist in selecting the best possible treatment. This is important as the severity of the condition normally over time and requires adjustment of the treatment to fit the patient’s case. Overall, asthma will need to be categorised based on four main groups; Severe persistent, moderate persistent, mild persistent, and mild intermittent. The four described in the table below.
Figure 1. Classification of asthma
To rule out the possibility of other conditions like chronic obstructive pulmonary disease (COPD) and respiratory infections, the child will be undertaken through a lung (pulmonary) function tests to establish the extent to which the child inhales and exhales air while breathing (Ahmed et al. 2016). The patient will also be undertaken through a spirometry test to determine the extent to which his bronchial tubes have narrowed by examining the amount of air that he can exhale whenever he takes a deep breath and the rapidity of his exhalation (MayoClinic, 2019). A peak flow meter will also be used to determine the degree of difficulty the child experiences while breathing out. To this extent, abnormally low peak flow readings would indicate that the child’s lungs may not be working properly and that asthma may have worsened (MayoClinic, 2019).
Nursing diagnosis
Constant coughing and poor airway clearance
- An increase in the production of mucus and retention of secretion
- Constant wheezing
- Dyspnea
- Impaired patterns of breathing
Constant fatigue during slight exercises
- Accretion of fluid in lungs 9 (Ahmed et al., 2016).
Goal
Ensure that the child’s airways become effective – The basis of this goal is controlling the inflammation in the airways and minimising the child’s exposure to allergens to enable normal respiratory processes.
Outcome
- The child experiences increased gaseous exchange.
- The child experiences a natural and effective cough.
- The child does not experience wheezing, or strange breathing sounds
- The child demonstrates diminished viscosity of secretions (Ahmed et al., 2016).
Interventions
- Educate or teach the child’s parents on the right techniques for controlling cough.
- Assess the level of consistency of sputum as well as the colour and quantity of sputum
- Provide oral care as well as teach the child’s parents on how to perform the cleanliness.
- Teach the parents of the client and the client on how to reduce the viscosity of secretions.
- Perform suction after listening to the sounds of the child’s lungs via auscultation.
- Carry out chest physiotherapy methods with postural drainage, chest percussion, and fibrosis.
For the treatment of asthma, the treatment goals include managing the inflammation in the airways and restricting or totally preventing exposure to a substance known to trigger the symptoms (Skoner, 2002). Building on McGill’s nursing model, it is determined that asthma treatment will need to be collaborative, and would, therefore, involve teamwork between healthcare practitioners, the patient diagnosed with asthma, and the family of the patient.
The main types of medications vary from the use of control drugs for purposes of preventing asthma attacks and rescue to the use of quick-relief drugs that are particularly vital during an asthma attack (Skoner, 2002). As an alternative, long-term control drugs should be used in an attempt to prevent or manage symptoms in asthma patients – particularly patients experiencing moderate to severe symptoms of asthma.
Common examples of these groups of drugs (long-term control drugs) include inhaled steroids for inhibiting symptoms by preventing the swelling of the airways. Conversely, quick-relief drugs are designed for relieving and controlling the symptoms and have to be used in the event of an asthma attack, particularly when a patient continually wheezes or coughs. Typical examples of this group of drugs include short-acting bronchodilators like in the case of Proventil and Ventolin (Skoner, 2002).
Rationale
- The sputum characteristics will be used to determine the extent of the airway obstruction (Carr et al., 2017; Fahy & Dickey, 2010).
- Constant coughing will need to be controlled, as it can lead to the child’s exhaustion, frustrate the child, and trigger depression (Carr et al., 2017).
- Secretions may lead to a blockage of mucus, contributing to an occurrence of atelectasis (Carr et al., 2017)
- Controlled additional noises in the child’s breathing would indicate success in ensuring that the airways can effectively breathe.
- Ensuring oral hygiene in the child is necessary, as it will check against bad breath 9 (Ahmed et al., 2016).
Safety Considerations
- Develop a comprehensible written plan with the support of the child’s parents on how the child’s medication will be managed.
- In case the child is hospitalised, constantly communicating the medical decisions in relation to the child’s health progress will be undertaken through the parents, or any other available caregiver (Lacey, Janis & Cox, 2008).
Developmental Considerations
The idea of coming up with the child’s asthma action plan collaboratively with his parents or caregivers is crucial, as it will facilitate effective asthma management (Miles et al., 2017). The very vital pointers to put into account to encourage positive health progress of the child include:
- Developing a written plan with details on when and how the medications will be taken.
- Instructing the child’s parents or caregivers on how to carry out quick relief interventions and long-term control medications in case a need arises.
- Coming up with a list for actions to be pursued in the control of the client’s environment
- Educating the parents and the child on how to eliminate typical attack triggers, such as irritants, allergens, or colds (Skoner, 2002).
Communication with the family and child
When it comes to communicating with the child, it is recommended that dyadic communication should be used. There are several reasons for this. This type of communication is critical, as it would enable the child to talk freely and to interact without restraint via a face to face method with the healthcare practitioners (Gavron & Mayseless, 2018; Shafi et al., 2019). Close interaction with the patient is considered to be vital, particularly as it facilitates an efficient childcare consultation (Mazuz, 2013). The process will entail facilitative a collaborative and interpersonal relationship with the child to encourage him to communicate freely while disclosing some vital signs characterising his condition d (Staa, 2011). This will assist in developing an effective asthma management plan that is customised to the patient.
As regards communicating with the child’s family or caregivers, it is proposed that triadic communication should be used, particularly as it will enable a three-way communication among three groups of people of interest: healthcare practitioner, the child patient, and the child’s family members or caregivers (Jeon & Myers, 2017). This kind of communication will be crucial for the child’s case owing to its capacity to facilitate the development of therapeutic alliances in the processes of asthma review consultations (Lacey et al. 2008). Technically, a healthcare practitioner will need to encourage the involvement of the child, and the child’s parents or caregivers in the communication cycle. This type of communication is found to be useful for the child’s case, as it would provide the child with a chance to freely talk about his existent conditions and concerns with the supervision of their parents (Cahill & Papageorgiou, 2007). The parents will also have an opportunity to discuss the child’s condition and their concerns, as well as provide them with an opportunity to make important decisions relating to the forms of interventions that consider appropriate (Callery, 2013).
Impact of hospitalisation on child and family
- A very likely impact of hospitalisation on the child include, the child indicating a regress in behaviour and demonstrating indifference to activities that demand some degree of physical strain (Staa, 2011).
- The child may demonstrate a greater level of dependence on his family members to undertake normal tasks, like wearing a sweater, or even being put to bed.
- It is also likely that the child may experience degradation in the areas of social and educational development because of failure to attend school as frequently as other children (Effgen, 2012).
- Separating the child from the family as a result of the child’s hospitalisation may contribute to the child’s agony by negatively affecting a close attachment to his family members (Callery, 2013).
ORDER NOW HERE
Discharge Planning/Teaching
The idea of having a discharge planning is critical, owing to a need to make sure that the patient is provided with the required frequency and degree of medical attention to prevent the child’s re-hospitalisation (Lacey et al., 2008). The strategies that would come in handy in this area include:
- Overseeing patient referral with the community health services, particularly a physical therapist. This will ensure that an optimal control is achieved in asthma management (Price et al., 2017).
- Creating explicit training plans in collaboration with the child’s parents or caregivers. Pertinent strategies that are critical in this specific area includes training the child’s parents and caregivers on how to manage the child’s symptoms in case of emergencies, including by making use of suctioning techniques and reading glucometer (Lacey et al., 2008).
- Initiating discharge planning procedures, including working collaboratively with concerned healthcare practitioners to see to it that all strategies included in the plan are followed appropriately before eventually discharging the child.
- Confirm that the child has been provided with the required devices for home nursing or care, and that future outpatient appointment is made in advance (Callery, 2013).
Evaluation
The child’s airwaves will need to be assessed during the pre-arranged outpatient appointments. The key areas to be examined during these visits will include the extent of the airwave obstruction and inflammation, increase or decrease in the child’s gaseous exchange, the ease with which the child coughs, any occurrence of wheezing or related absurd breathing, and whether the level of viscosity of the child’s secretion has reduced (Callery, 2013).
Conclusion
McGill’s nursing model has been applied in this nursing care plan to develop and assess a plan for health promotion for a child who has been diagnosed with asthma. Target outcomes are improved gaseous exchange, ease in coughing and reduced viscosity of secretions. I believe that having such a care plan is significant, as it would facilitate a continual, consistent, and efficient collaborative understanding of an asthmatic child’s care history, communication across departments in the hospital, and decision-making regarding the type of care suitable for the child. This will have significant implications on my professional development by enabling me to make sure that the safety, continuity, and care of the patient is consistent both at home among the family members and in the hospital among healthcare practitioners. In my opinion, it would provide me with a sense of direction regarding the type of nursing care the child would and his family would need. I engaged in a lot of research in the process of developing the care plan. This enabled me to understand that at the core of a nursing care plan should be to encourage evidence-based, standardised, and holistic care. Hence, it is more than just a tool containing priority problems to a certain patient, as it also contains evidence-based nursing directives directly related to interventions to the problems.
References
Ahmed, S., Ernst. P., Barlett, S. et al. (2016). The Effectiveness of Web-Based Asthma Self-Management System, My Asthma Portal (MAP): A Pilot Randomized Controlled Trial. J Med Internet Res, 18(12), 313.
Barnes, P. (2006). Pathophysiology of Asthma. Ch 5. London: National Heart and Lung Institute,
Bhattacharjee, S., Haldar, P., Maity, S. & Debnat, S. (2018). Prevalence and Risk Factors of Asthma and Allergy-Related Diseases among Adolescents study: rationale and methods. ERJ Open Res, 4, 34-201
Cahill, P., & Papageorgiou, A. (2007). Triadic communication in the primary care paediatric consultation: a review of the literature. The British Journal Of General Practice, 57(544), 904–911.
Callery P. (2013). Communicating with children with asthma. Nursing Times, 109(7), 22-23
Carr, T. F., Altisheh, R., & Zitt, M. (2017). Small airways disease and severe asthma. The World Allergy Organization journal, 10(1), 20.
Doenges, M., Moorhouse, M. & Murr, A. (2019). Nursing Care Plans: Guidelines for Individualizing Client Care Across the Life Span. Philadelphia: F.A. Davis..
Effgen, S. (2012). Meeting the Physical Therapy Needs of Children. Philadelphia: F.A. Davis.
Fahy, J. V., & Dickey, B. F. (2010). Airway mucus function and dysfunction. The New England journal of medicine, 363(23), 2233–2247.
Gavron, T., & Mayseless, O. (2018). Creating Art Together as a Transformative Process in Parent-Child Relations: The Therapeutic Aspects of the Joint Painting Procedure. Frontiers in psychology, 9, 2154.
Promoting Health and Preventing Ill Health Essay Paper