Resistance In African Anopheles Mosquitoes Essay
Resistance In African Anopheles Mosquitoes Essay
Question:
Discuss About The Resistance In African Anopheles Mosquitoes?
Answer:
Introduction
The brochure focuses on the causative agent of the African malaria (Anopheles gambiae). It is considered as the most efficient vector of malaria in the Afrotropical region (CDC 2010). It mainly composed of eight isolated reproductive species that cannot be distinguished morphologically. This brochure will focus on some of the recent findings regarding Anopheles gambiae aiming to reduce its ill effect.
Audience
The audience of this brochure is group of people who have been suffering from African malaria or for the researchers who are keen to do research or gain knowledge about the recent researches in this field.
The purpose of this brochure is to give an understanding on the current findings on Anopheles gambiae, its host pathogen interaction in the midgut that is responsible for the infection. The brochure would further provide the knowledge how the mosquitoes are gaining resistance over the insecticides and the recent recommendations.Resistance In African Anopheles Mosquitoes Essay. It also provides an in depth knowledge about the components of some natural essential oils containing repellant property and also provides with the information regarding the tribal traditions of using herbs and plants to prevent the vectors.
Annotated Bibliography
Boissière, Anne, et al. “Midgut microbiota of the malaria mosquito vector Anopheles gambiae and interactions with Plasmodium falciparum infection.” PLoS pathogens 8.5 (2012): e1002742.
The vulnerability of the Anopheles mosquito to the plasmodium infections depends mainly on the complex interaction between the vectors and the malarial parasite. a number of studies have referred to the fact the mosquito poses an immunity to control the malarial infection, but very little is known about the role of the environmental factors in the process of transmission.
It has been found that it is the gut microbiota that is actually responsible for the mosquito infection. A. gambiae mosquitoes were isolated from Cameroon and were experimentally challenged with P. falciparum isolate and the bacterial content of the gut is subjected to
Malaria control is reliant on insecticides to control the mosquito vector. As efforts to control the disease have intensified, so has the selection pressure on mosquitoes to develop resistance to these insecticides. The distribution and strength of this resistance has increased dramatically in recent years and now threatens the success of control programs. This review provides an update on the current status of resistance to the major insecticide classes in African malaria vectors, considers the evidence that this resistance is already compromising malaria control efforts, and looks to the future to highlight some of the new insecticide-based tools under development and the challenges in ensuring they are most effectively deployed to manage resistance.
Uganda’s malaria burden includes the sixth highest number of annual deaths in Africa (10,500) with approximately 16 million cases (2013) and the entire population at risk. Resistance In African Anopheles Mosquitoes Essay. The President’s Malaria Initiative has been supporting the malaria control interventions of indoor residual spraying (IRS) and distribution of long-lasting insecticidal nets (LLIN) in Uganda since 2007. These interventions are threatened by emerging and spreading insecticide resistance, known to exist in Ugandan malaria vectors. Pyrethroid insecticides have been used in agriculture since the early 1990s and in IRS programmes from the mid-2000s until 2010. A universal LLIN coverage campaign was executed in 2013–2014, distributing pyrethroid-treated LLINs throughout the country. This study investigated insecticide susceptibility, intensity, and oxidase detoxification in Anopheles gambiae sensu lato and Anopheles funestusto permethrin and deltamethrin in four eastern Ugandan sites.
Methods
The susceptibility status of An. gambiae and An. funestus to bendiocarb, permethrin and deltamethrin was determined using the CDC (Centers for Disease Control and Prevention) bottle bioassay. Presence of oxidative enzyme detoxification mechanisms were determined by pre-exposing mosquitoes to piperonyl butoxide followed with exposure to discriminating doses of deltamethrin- and permethrin-coated CDC bottles. Resistance intensity was investigated using serial dosages of 1×, 2×, 5× and 10× the diagnostic dose and scored at 30 min to determine the magnitude of resistance to both of these LLIN pyrethroids. Testing occurred in the Northern and Eastern Regions of Uganda.
Results
Anopheles gambiae and An. funestus were fully susceptible to bendiocarb where tested. Anopheles gambiae resistance to deltamethrin and permethrin was observed in all four study sites. Anopheles funestuswas resistant to deltamethrin and permethrin in Soroti. Oxidative resistance mechanisms were found in An. gambiae conferring pyrethroid resistance in Lira and Apac. 14.3% of An. gambiae from Tororo survived exposure of 10× concentrations of permethrin. Resistance In African Anopheles Mosquitoes Essay.
Conclusions
Both An. gambiae and An. funestus are resistant to pyrethroids but fully susceptible to bendiocarb at all sites. Susceptibility monitoring guided the Ministry of Health’s decision to rotate between IRS insecticide classes. Intensity bioassay results may indicate encroaching control failure of pyrethroid-treated LLINs and should inform decision-makers when choosing LLINs for the country.
Background
Renewed interest in malaria elimination has led to the scale-up of vector control measures in sub-Saharan Africa (SSA) [1]. Given that IRS and LLINs, the most effective malaria prevention methods, rely heavily on insecticide use, it is critical to monitor vector resistance to insecticides [2]. Both LLINs and IRS are the priority malaria prevention interventions in Uganda. Uganda attempted a universal LLIN coverage campaign (one LLIN per two people) in 2014 after distributing over 22 million LLINs provided by the Global Fund to Fight AIDS, Tuberculosis and Malaria (GFATM), USAID/PMI, World Vision and other partners, distributing LLINs over most of the country. With support from USAID/PMI and the Department for International Development (DFID), IRS was implemented in 10 districts in northern Uganda from 2007 to 2014 and is currently performed in 14 new highly malaria-endemic districts in northern and eastern Uganda. All these expanded vector control measures coupled with use of pesticides in agriculture exert insecticidal pressure on local malaria vector mosquitoes, which may accelerate the development and spread of insecticide resistance. Past studies conducted in Uganda have confirmed that Anopheles gambiaesensu lato (hereafter An. gambiae) was susceptible to carbamate and organophosphate insecticides, however, pyrethroid resistance was detected in Apac, Lira, Soroti and Tororo District surveillance sites, although there was wide variation in susceptibility to the different pyrethroids. Pyrethroid and dichlorodiphenyltrichloroethane (DDT) resistance in both An. gambiae and Anopheles funestus is a growing problem in the country [3,4,5,6,7,8,9] and has become a major malaria control concern and a threat to the success of insecticide-based malaria vector control programmes, not only in Uganda, but in most of sub-Saharan Africa (SSA) [10,11,12]. Insecticide resistance will definitely affect the achievement of the goal of Uganda National Malaria Control Programme (NMCP) for “A Malaria Free Uganda” [13, 14]. Resistance In African Anopheles Mosquitoes Essay. Thus, insecticide resistance management is presently one of the main focus areas of the WHO Global Malaria Programme [15].
In Uganda, the level of An. gambiae vector resistance against bendiocarb, deltamethrin and permethrin was investigated in four sites (Apac, Lira, Soroti and Tororo Districts) that are located in highly malaria-endemic rural areas of northern and eastern Uganda [16]. These four sites are situated in and next to the present-day IRS operational zone. The CDC bottle bioassay [17, 18] was used for determining insecticide resistance status, mechanisms and intensities in the major malaria vectors An. gambiae and An. funestus to three public health insecticides used for IRS, two of which are used in the impregnation of LLINs. Two of the current surveillance sites, Apac and Tororo, were also a part of the national malaria vector resistance studies conducted by the MoH and Malaria Consortium using WHO tube bioassays [19, 20] in 2009 and by MoH and Abt Associates in 2011, 2013 [3] and 2015.
This paper presents the findings of recent studies on the insecticide susceptibility status of An. gambiae. and An. funestus against bendiocarb, deltamethrin and permethrin in Apac, Lira, Soroti and Tororo.
Methods
Study sites
The study was conducted in Lira and Tororo (current IRS districts), Apac (former IRS district) and Soroti (a non-IRS district), all rural districts (Fig. 1). Apac, Lira, and Soroti Districts are north and northeast of Lake Kyoga in northern Uganda and Tororo District is in southeast Uganda along the Kenyan border (Fig. 1). Apac, Lira, and Soroti Districts consist of mostly flat country with small, scattered rolling hills with rock and boulder outcroppings. Savannah woodland with swamps and wetlands are common in these three districts with villages dispersed throughout. Tororo District is hilly over much of the countryside and Tororo town has a volcanic core within city limits. Tororo District large boulders scattered throughout; the Kenyan highlands are to the east and visible from town. Riverine zones and lowlands in Tororo District are planted in rice.
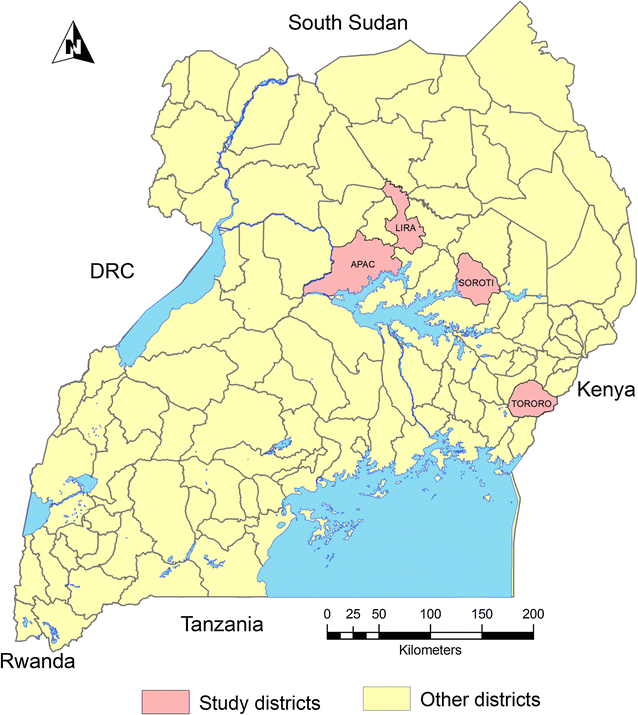
Map of Uganda showing susceptibility assay study districts
Apac District is located approximately 262 km north of Kampala, the capital city of Uganda. Apac lies between longitudes 32° E and 34° E and latitudes 2° N and 3° N, at an average altitude of 1150 m above sea level with 9% of the district consisting of open swamps. Lira District is located approximately 364 km north of Kampala and lies between latitudes 1° 21′N and 2° 42′N and longitudes 32° 51′E, 34° 15′E, at an average altitude of 1200 m above sea level. Soroti District is located 347 km northeast of Kampala and lies between longitudes 30° 01′E and 34° 18′E and latitudes 1° 33′N and 2° 23′N, at an average altitude of over 1250 m above sea level. Tororo District is located 205 km northeast of Kampala and lies between 0° 45′N, 34° 5′E in Eastern Uganda on the Kenyan border. Resistance In African Anopheles Mosquitoes Essay.
All four districts have stable, perennial malaria transmission with malaria prevalence rates ranging from 37 to 63% [21]. All sites experience two malaria peaks following two rainy seasons which occur from March to May and again from August to October with intermittent rain in-between. Annual rainfall totals range from 1200 to 1800 mm. Temperatures in northern Uganda (Gulu climate data) range from an average monthly high of 25 °C in February to a low of 22.3 °C in July [22].
Study district populations according to the National Population and Housing Census (2014) are Apac, 368,000; Lira, 408,000; Soroti, 297,000; and Tororo, 517,000. All district populations are > 75% rural. Three types of house predominate in these districts: permanent houses with plastered and painted wall surfaces, semi-permanent houses with mud and wattle walls and tin roofs, and temporary houses with mud and wattle walls and thatch roofs that make up the majority of houses in all districts. Major agricultural products in all test districts include sweet potatoes, cassava, groundnuts, beans, maize, millet and sorghum, and other recently introduced crops such as rice, sunflower, soybeans, and citrus fruit. Horticultural crops serve both as food and cash crops. Livestock, mainly cattle, goats, sheep, rabbits, swine, and poultry are raised [23].
Mosquito collections
Anopheline mosquitoes were collected from larval breeding sites or as adults from indoor resting collections in Apac, Lira, Soroti and Tororo (Fig. 1).Resistance In African Anopheles Mosquitoes Essay. Trained mosquito collectors used test tubes to collect indoor resting mosquitoes between 5.00 a.m. and 7.00 a.m. in June 2015 following a verbal consent from house owners. Larvae were collected from different types of breeding habitats (roadside ditches, marram/brick/sand pits, ponds, puddles, hoof prints) using dippers/scoops and reared in an insectary at 28 ± 2 °C room temperature and 75–80% relative humidity. Individual adult Anopheles mosquitoes collected from the field were identified using a simplified morphological key adapted from Gillies and Coetzee [24].
Insecticide susceptibility tests
The CDC bottle bioassay [17, 18] was used for detecting resistance to insecticides. The bioassay is, in principle, the same as the WHO paper tests [19, 20]. Morphologically identified non-blood fed 2–5 day old An. gambiae and An. funestus adult mosquitoes were tested with the standard CDC bottle bioassay using diagnostic doses of 12.5 and 21.5 μg/bottle of deltamethrin and permethrin, respectively at a diagnostic time of 30 min applicable to Anopheles mosquito populations [25]. The study teams treated bottles using diluted insecticide prepared and brought from CDC Atlanta. Four replicates (bottles) of approximately 25 mosquitoes served to monitor susceptibility status with another 10–15 added to a fifth acetone-only treated control bottle. The diagnostic dose for each insecticide was determined as the minimal amount of an insecticide needed to kill all susceptible mosquitoes at 30 min. A 30 min exposure in treated bottles is considered the most critical value, because it represents the threshold between susceptibility and resistance. Mosquitoes were considered dead when they could no longer stand, were immobile, and slid along the curvature of the test bottle. Mortality was recorded every 15–120 min, if necessary, for treated-bottle survivors. At the end of 120 min, control bottle mortality was scored [18]. Resistance In African Anopheles Mosquitoes Essay.
Insecticide resistance mechanism tests
Insecticide resistance mechanisms were investigated with a synergist, piperonyl butoxide (PBO), in An. gambiae and An. funestus to two insecticides commonly used in Uganda malaria control programme interventions: deltamethrin (IRS and LLINs) and permethrin (LLINs) [17, 18]. Oxidase (P450) resistance mechanisms were determined by pre-exposing An. gambiae and An. funestus to the oxidase inhibitor PBO at 50 μg/bottle for 1 h, followed immediately with exposure to discriminating doses of deltamethrin and permethrin-coated CDC bottles at 12.5 and 21.5 μg/bottle, respectively, for 30 min [25]. Resistance and intensity testing were not performed with carbamate insecticide, to which test mosquitoes were fully susceptible.
Insecticide resistance intensity tests
Insecticide resistance intensity testing of An. gambiae and An. funestusto permethrin and deltamethrin was performed by exposing them to CDC bottles coated with serial dosages, first at the diagnostic dosages of 12.5 and 21.5 μg/bottle of deltamethrin and permethrin, respectively, and subsequently to doses of 2×, 5× and 10× the diagnostic dosages. The test bottles and insecticide concentrates were prepared and provided by CDC staff in Atlanta, Georgia, USA, developers of the CDC bottle bioassay method. One bottle was prepared for each concentration; approximately 25 mosquitoes were exposed to each diagnostic dose and each test included a control bottle of 10–15 mosquitoes.
ORDER A PLAGIARISM-FREE PAPER NOW
Interpretation of results of insecticide susceptibility tests
All mosquitoes that die within the diagnostic time period (30 min) when exposed to insecticide-coated bottles are susceptible to a tested insecticide. Test mosquitoes surviving beyond the diagnostic time threshold are assumed to have some degree of resistance. The most important information is the mortality at the diagnostic time, but the bioassay is monitored beyond the diagnostic time to evaluate the percentage of resistant mosquitoes. Interpretation of CDC bioassay results at 30 min is that < 95% mortality indicates resistance whereas WHO tube bioassays score suspected resistance at 90–97% and confirmed resistance at < 90% mortality [17, 20]. Resistance In African Anopheles Mosquitoes Essay. CDC bioassay tests are discarded if control mortality is > 10%. Abbott’s formula is used to correct results if the mortality at 2 h in the control bottle is between 3 and 10% [26].
Determining insecticide resistance mechanisms
Increased production of detoxification enzymes in target insects can play an important role in insecticide resistance [17, 18]. Pre-exposing an insect to an enzyme inhibitor (synergist) will often overcome a targeted metabolic resistance mechanism and return such insects to near full susceptibility to a particular insecticide. Three outcomes are seen after testing: (a) return to full (or near full) susceptibility to the insecticide in the CDC bottle bioassay after pre-exposure to the synergist; (b) if resistance to the insecticide is only partially abolished then the metabolic mechanisms related to the synergist are only partially conferring the resistance and other mechanisms may also play a role; and (c) if resistance to the insecticide does not change with pre-exposure to the synergist (i.e., an increase in mortality is not observed), the metabolic mechanisms related to the synergist are likely not involved in the resistance observed [17].
Determining insecticide resistance intensities
Resistance intensity testing is a relatively new procedure in use with the CDC bottle bioassay. Interpretation of tests demonstrating mosquito survival at 5× and 10× doses have yet to be correlated with control failure in association with LLIN or IRS use, but studies are underway to determine to what degree high intensity survival of field-collected mosquitoes is associated with operational failure. Resistance In African Anopheles Mosquitoes Essay.
